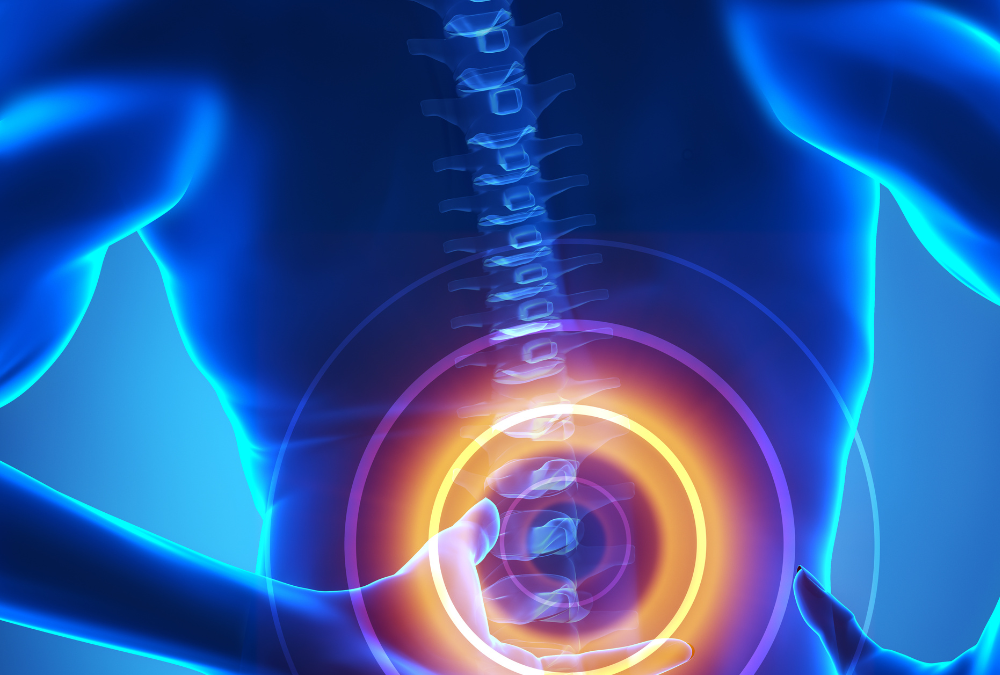
If I had a nickel for every back pain and sciatica patient that told me they had a slipped disc, I could retire. After all, low back pain causes more missed workdays than any other condition world-wide, making it the largest cause of disability. Many factors can give you back pain, from poor posture and muscle strains to serious medical conditions, but the most common fear I get from my low back patients is whether they have a slipped disc. I cannot fault these patients, because google searches for low back pain symptoms tend to assume the worst, and herniated discs top the results list. Luckily for us—especially my patients—a slipped disc often isn’t the cause of the back pain and even in cases where we suspect a disc injury, we can still do a lot for the pain.
What is a “Disc?”
One of my physio mentors told me to think of a disc like one of the ketchup packets you get at McDonald’s. This essentially captures how discs work: fluid-filled packets that sit between your spine segments, cushioning and spacing them out. A herniated disc, also known as a slipped disc or a ruptured disc, occurs when the soft inner core of a spinal disc pushes through a crack in the tougher outer layer, creating a bulge that can put pressure on a nerve. This can cause pain, numbness, or weakness in the area where the affected nerve travels.
Imagine pushing on one end of a ketchup packet—actually try it if you have one handy—and note what happens. The fluid gathers on the other end, creating a bulge. In your spine, this bulge can push out and put pressure on a nerve, causing pain in your back, hips, and throughout your entire leg.
Why does my leg hurt if the problem is in my back?
I always tell my sciatica patients to picture a child stepping on a garden hose. Now imagine trying to water your garden—no luck, right? Now think of the painful part of your leg like the frustrated gardener. Whenever a structure such as a disc, joint or muscle pushes on a nerve, it can interfere with the flow of nerve signals and other fluids that keep the nerve healthy. This causes irritation and pain in the area the nerve travels to. Of all the nerves that travel from your back into your leg, the largest and most affected nerve is your sciatic nerve: hence the name sciatica. The solution: get the child off the hose!
So it’s not necessarily a disc?
While herniated discs can create significant discomfort, the disc itself doesn’t always cause the pain and just because you have a herniated disc doesn’t mean you’ll feel pain. Some research suggests that many of us (over 50%) would likely show a disc herniation at some level and not feel any back pain at all.
Many other structures around your spine can give you back pain, such as the joints between your spinal segments and your lower back muscles. Some studies have linked back pain to other factors such as muscle strains, muscle imbalances and posture. The key to fixing the problem lies in a comprehensive assessment and diagnosis. In other words, you need to figure out whether it is indeed a child standing on your garden hose and where along the hose the child is standing. In every case, regardless of whether the pain is caused by a herniated disc, arthritis or other joint or muscle issue, patients almost always end up with a comprehensive strengthening and mobility program.

What if it is a disc?
So, you’ve had a thorough assessment and your physiotherapist decides they can’t rule out a disc issue–now what? I chose my words very carefully in that last sentence, as the only way to definitively diagnose you with a disc issue is to confirm with an MRI, getting an appointment for which–where I live and work–can take months, a frustrating wait. For this reason, I tell my patients that while I can’t definitively diagnose them with a herniated disc until the MRI, we can begin to treat them with the assumption that a disc herniation is present.
What does that mean? My initial approach focuses on reducing pain, improving mobility, and strengthening the surrounding muscles to support the spine through targeted exercises, manual therapy, and other treatment modalities. I also educate patients on proper body mechanics, ergonomics, and techniques to avoid flaring up their symptoms while we strengthen and condition around the spine. In many cases, by the time the MRI appointment comes around, my patients tell me their back feels almost back to normal, even if their MRI still picks up a herniated disc–wild, right?
Get Your Roar Back
What does physiotherapy back pain assessment look like?
I typically spend 45 minutes to an hour on each new back pain patient. A large portion of this time is actually spent in conversation, as taking a thorough history is a vital part of any low back pain assessment. Here, I’m interested in things such as:
• What you do for work and fun
• Your medical history
• How your back pain began and what makes it worse
• Your daily routine • Your activity and performance goals
I follow this up with a physical examination, where I take an in-depth look at how you move, stand, sit and walk. This encompasses things like:
• Your range of motion and mobility
• Your reflexes
• Your gait and sitting/standing posture
• Special Tests
• Your overall muscle strength
Every initial low back pain assessment includes treatment where I begin to treat the patient’s symptoms and try to help them move better. I use a variety of methods, such as manual therapy, spinal mobilization, dry needling and soft tissue techniques alongside developing a comprehensive home exercise program. My patients can often expect up to 50-70% improvement in their low back pain symptoms within the first session.
Prevention of future back injuries
In addition to providing relief and restoring functionality, back pain physiotherapy also focuses on preventing future injuries. I always educate my patients on proper body mechanics, ergonomics, and techniques to protect the spine during daily activities. By learning how to move correctly and strengthening the muscles that support your lower back, you can significantly reduce the risk of future back pain episodes. Physiotherapy empowers you to take an active role in your health and well-being, leading to long-term benefits and a reduced likelihood of recurring low back pain.
Conclusion
Back pain can significantly impact your life, keeping you from your work, play and even your loved ones, but it doesn’t have to be permanent. Back pain physiotherapy offers a holistic approach to managing and treating back pain, focusing on pain relief, improved mobility, and prevention of future injuries. By working with a physiotherapist, individuals can regain control over their lives and find long-term relief from back pain. So, if you struggle with back pain, consider trying physiotherapy and experience the benefits for yourself.
Love this!! Super helpful and really informative would love to see the research you’ve used to make this amazing blog in future blogs !! –